|
Rassegna Stampa Scientifica Agosto 2022
|
State of the Art Review
Impact of vaping on respiratory health
BMJ 2022;378:e065997 (Published 18 July 2022)
Andrea Jonas
https://www.bmj.com/content/378/bmj-2021-065997
Breaking Nicotine’s Powerful Draw
Millions of smokers could be forced to confront the agony of nicotine withdrawal as the F.D.A. weighs calling for a drastic reduction in the addictive lure of cigarettes.
Aug. 2, 2022
At some point in the next few years, the 30 million smokers in the United States could wake up one day to find that cigarettes sold at gas stations, convenience stores and smoke shops contain such minuscule amounts of nicotine that they cannot get their usual fix when lighting up.
Would the smokers be plunged into the agonizing throes of nicotine withdrawal and seek out their favorite, full-nicotine brand on illicit markets, or would they turn to vaping, nicotine gum and other less harmful ways to get that angst-soothing rush?
Such scenarios inched closer to the realm of possibility in June, when the Food and Drug Administration said that it would move toward slashing nicotine levels in cigarettes in an effort to reduce the health effects of an addiction that claims 480,000 lives a year.
The agency set next May as its timetable for introducing a fully developed proposal. But many experts hope regulators will champion an immediate 95 percent reduction in nicotine levels — the amount federally funded studies have determined is most effective for helping smokers kick the habit.
It could be years before any new policy takes effect, if it survives opposition from the tobacco industry. Even so, health experts say any effort to decrease nicotine in cigarettes to nonaddictive levels would be a radical experiment, one that has never been implemented by any other country.
The science of nicotine addiction has come a long way since 1964, when a U.S. Surgeon General report first linked smoking to cancer and heart disease, although it would take another two decades for the mechanics of nicotine dependence to be understood and widely accepted.
Tobacco contains more than 7,000 chemicals, many of them harmful when burned and inhaled, but it is nicotine that keeps smokers coming back for more. Nicotine stimulates a surge of adrenaline in the brain while indirectly producing a flood of dopamine, the chemical that promotes feelings of contentment and relaxation. The effects, however, are short-lived, which is why heavy smokers need a fresh injection a dozen or more times a day.
Eric Donny, a tobacco expert at Wake Forest University School of Medicine who has conducted experiments with low nicotine cigarettes, says many scientists have come to embrace a 95 percent reduction in nicotine levels as ideal for helping study subjects smoke less. Anything higher, he said, can encourage participants to engage in so-called compensatory smoking — inhaling more deeply or smoking more frequently.
The studies he and other scientists have run recently used genetically modified tobacco bred to express less nicotine; bringing nicotine down to zero is not an option under the Tobacco Control Act, a 2009 law that gave the F.D.A. the power to regulate the manufacture and marketing of tobacco.
“When you get the nicotine in tobacco low enough, you just can’t get enough nicotine to maintain the dependence,” Dr. Donny said. “Smoking more creates adverse effects, like nausea, because the lungs can only handle so much of a burned substance.”
But even as tobacco control researchers cheered the F.D.A. announcement, they acknowledged that any move to lower nicotine in cigarettes would be enormously challenging for inveterate smokers — even among the 70 percent who have said they would like to stop. As it is, fewer than one in 10 adults who try to quit smoking succeed, a reflection of nicotine’s addictive prowess and the limitations of nicotine replacement therapy.
Dr. Nora Volkow, director of the National Institute on Drug Abuse, expressed confidence in the studies that backed an immediate cut in nicotine levels versus a gradual tapering. But she said that scientists and regulators still needed to address the welter of unforeseen consequences that could prove disruptive to determined smokers and could fuel the creation of underground markets for full-nicotine cigarettes. “You cannot completely predict outcomes based on a clinical randomized study,” she said. “Biology and life are not so precise.”
Some scientists have urged caution for any plan that would drastically cut nicotine levels in one fell swoop, warning that the existing research on low-nicotine cigarettes is imperfect, given the high number of study participants who cheat. The skeptics, among them tobacco company executives, warn that banning conventional cigarettes would drive determined smokers to seek imports from Mexico and Canada. They also argue that some smokers, including teenagers, could develop a habit that pairs vaping or nicotine gum with low-nicotine cigarettes, which are just as carcinogenic as traditional cigarettes.
Lynn T. Kozlowski, a tobacco researcher at the University at Buffalo who has contributed to four Surgeon General reports on smoking since 1981, said nicotine was a highly addictive drug, with a stranglehold on users that could rival cocaine and heroin, and that the F.D.A. needed to consider how a sweeping decrease of nicotine in cigarettes would affect smoker behavior.
“What scares me is a national experiment with very low nicotine cigarette that is done without some testing in the real world,” he said. The studies many experts cite when promoting a 95 percent drop in nicotine levels relied upon paid participants, he noted, adding that some of them secretly smoked their own brands at the same time that researchers were plying them with low-nicotine cigarettes.
In interviews, smokers who had heard about the F.D.A.’s announcement said they were conflicted by the prospect of being forced to abandon their addiction, despite knowing full well that it damaged their health and would likely shorten their life span. Mike Harrigan, an options trader who was taking a smoking break outside the Chicago Board of Trade, said he feared he might actually end up smoking more if cigarettes contained significantly lower amounts of nicotine. “It may help newer smokers, but it will hurt people who are used to a certain level of nicotine,” said Mr. Harrigan, 55, who has been a pack-a-day smoker for three decades.
Dr. Kozlowski said he was especially concerned by the agency’s mixed messaging and seemingly conflicted stance on e-cigarettes, which deliver nicotine without the tar and many other toxins that are inhaled when tobacco is ignited. Even if the long-term impacts of vaping remain unknown — though health experts agree that teenagers should be discouraged from trying e-cigarettes — there is mounting consensus that such products are useful for helping adult smokers quit.
The F.D.A. has so far approved just six vaping products and has denied more than a million others, including those made by Juul Labs. Earlier this summer, the agency ordered Juul off shelves, citing the potential harm from chemicals that could leach out of its e-liquid cartridges. But the F.D.A. has since granted the company further review.
Dr. Judith Prochaska, an addiction specialist at Stanford University who runs a smoking cessation clinic for patients with cancer and their families, said lighting up during a stressful phone call, while sipping a cocktail or following a meal creates a powerful memory that conditions the mind into associating a cigarette with the stimulation or succor that it delivers via the rush of nicotine.
“All these everyday behaviors cue your brain that nicotine is coming,” she said. “It’s basically the Pavlovian dog effect but conditioned here with a highly addictive drug.”
Over time, the dependency deepens. Regular smoking promotes the formation of additional dopamine receptors — sometimes millions more. When a smoker goes cold turkey, those unrequited receptors prompt the anxiety, irritability and depression that can make nicotine withdrawal so hard to bear.
Nicotine patches, gum and vapes can help to satisfy some of the cravings, but they cannot replace the rituals of having a cigarette: the retreat outside with a co-conspirator, the crinkling of cellophane and foil as you open a new pack, the heady buzz of that first drag.
Bruce Holaday, 69, a retired educator from Mill Valley, Calif., knows full well the power of nicotine. Over the past five decades, Mr. Holaday reckons he has tried to quit 100 times, often relying on nicotine replacement products. But he invariably returned to his lifelong, pack-a-day affair with Marlboro Lights.
His last attempt in August, a cold turkey gambit without nicotine replacement therapy, triggered an excruciating maelstrom of cravings that lasted several months. “It was like a sudden earthquake of desire and need, and then there would be these tremors for the next 10 to 15 minutes,” he said.
But this time, Mr. Holaday joined a support group at Stanford Health Care, which introduced a powerful social component into his quest. He described the effect as “not wanting to let the team down” and said he learned to avoid stressful situations, like watching the news. He discovered that if he could face down the initial waves of craving, they invariably subsided.
In late June, he passed the one-year mark since taking his last drag.
He gained weight but no longer gets easily winded on hikes. And he is confident he will never go back to smoking.
Asked about the prospect of drastic government intervention to compel Americans to quit, Mr. Holaday paused and thought about the first puff he took a half-century ago as a college freshman. “Without that nicotine rush, I would have probably walked away and never smoked again,” he said. “It will be rough for smokers, but anything we can do to prevent a new generation from getting hooked is a good thing.”
Robert Chiarito contributed reporting from Chicago.
Andrew Jacobs is a health and science reporter, based in New York. He previously reported from Beijing and Brazil and had stints as a metro reporter, Styles writer and national correspondent, covering the American South. @AndrewJacobsNYT
A version of this article appears in print on Aug. 2, 2022, Section D, Page 1 of the New York edition with the headline: A Plan to Ease the Cravings of Smokers.
https://www.nytimes.com/2022/08/02/health/fda-nicotine-addiction.html
Person-years of life lost and lost earnings from cigarette smoking-attributable cancer deaths, United States, 2019
International Journal of Cancer
First published: 10 August 2022
Farhad Islami, Emily C. Marlow, Jingxuan Zhao, Daniel Wiese, Samuel Asare, Priti Bandi, Blake Thomson, Zhiyuan Zheng, Nigar Nargis, K. Robin Yabroff, Ahmedin Jemal
https://onlinelibrary.wiley.com/doi/full/10.1002/ijc.34217
Related coverage:
Smoking Still Ends 123,000 American Lives Each Year
Note: The information in the article accurately reflects the study findings, but the headline omits the reference to cancer deaths. The overall toll of tobacco-related mortality in the US is generally cited as 480,000 annual deaths.
“In this national cohort study of 17 073 children with neuroimaging outcomes, a significant association was found of early-age initiation of tobacco use with lower crystalized cognition composite score and impaired brain development in total cortical area and volume. Region of interest analysis also revealed smaller cortical area and volume across frontal, parietal, and temporal lobes… These findings suggest that youths vulnerable to e-cigarettes and tobacco products should be treated as a priority population in tobacco prevention.”
Longitudinal Assessments of Neurocognitive Performance and Brain Structure Associated With Initiation of Tobacco Use in Children, 2016 to 2021
JAMA Netw Open. 2022;5(8):e2225991.
August 10, 2022
Hongying Daisy Dai, Gaelle E. Doucet, Yingying Wang, Troy Puga, Kaeli Samson, Peng Xiao, Ali S. Khan
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2794988
Related JAMA Netw Open Commentary:
Understanding the Association of Childhood Tobacco Use With Neuropathological Outcomes and Cognitive Performance Deficits in Vulnerable Brains
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2794992
Note: Open Access.
“The FCTC [Framework Convention on Tobacco Control] offers a framework to interpret state obligations to progressively realize the human right to health, with Article 14 and its guidelines providing a basis to clarify state obligations to ensure that those addicted to tobacco receive cessation support. However, Article 14 implementation has been limited. The right to health provides an alternative basis under international law to recognize the inherent dignity of those addicted to tobacco, implement FCTC
obligations under Article 14 and facilitate state accountability.”
Could international human rights obligations motivate countries to implement tobacco cessation support?
Addiction
First published: 06 July 2022
Benjamin Mason Meier, Martin Raw, Donna Shelley, Chris Bostic, Anahita Gupta, Kelsey Romeo-Stuppy, Laurent Huber
https://onlinelibrary.wiley.com/doi/abs/10.1111/add.15990
Person-years of life lost and lost earnings from cigarette smoking-attributable cancer deaths, United States, 2019
International Journal of Cancer
First published: 10 August 2022
Farhad Islami, Emily C. Marlow, Jingxuan Zhao, Daniel Wiese, Samuel Asare, Priti Bandi, Blake Thomson, Zhiyuan Zheng, Nigar Nargis, K. Robin Yabroff, Ahmedin Jemal
https://onlinelibrary.wiley.com/doi/full/10.1002/ijc.34217
Related coverage:
Smoking Still Ends 123,000 American Lives Each Year
Note: The information in the article accurately reflects the study findings, but the headline omits the reference to cancer deaths. The overall toll of tobacco-related mortality in the US is generally cited as 480,000 annual deaths.
“In this national cohort study of 17 073 children with neuroimaging outcomes, a significant association was found of early-age initiation of tobacco use with lower crystalized cognition composite score and impaired brain development in total cortical area and volume. Region of interest analysis also revealed smaller cortical area and volume across frontal, parietal, and temporal lobes… These findings suggest that youths vulnerable to e-cigarettes and tobacco products should be treated as a priority population in tobacco prevention.”
Longitudinal Assessments of Neurocognitive Performance and Brain Structure Associated With Initiation of Tobacco Use in Children, 2016 to 2021
JAMA Netw Open. 2022;5(8):e2225991.
August 10, 2022
Hongying Daisy Dai, Gaelle E. Doucet, Yingying Wang, Troy Puga, Kaeli Samson, Peng Xiao, Ali S. Khan
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2794988
Related JAMA Netw Open Commentary:
Understanding the Association of Childhood Tobacco Use With Neuropathological Outcomes and Cognitive Performance Deficits in Vulnerable Brains
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2794992
Note: Open Access.
“The FCTC [Framework Convention on Tobacco Control] offers a framework to interpret state obligations to progressively realize the human right to health, with Article 14 and its guidelines providing a basis to clarify state obligations to ensure that those addicted to tobacco receive cessation support. However, Article 14 implementation has been limited. The right to health provides an alternative basis under international law to recognize the inherent dignity of those addicted to tobacco, implement FCTC
obligations under Article 14 and facilitate state accountability.”
Could international human rights obligations motivate countries to implement tobacco cessation support?
Addiction
First published: 06 July 2022
Benjamin Mason Meier, Martin Raw, Donna Shelley, Chris Bostic, Anahita Gupta, Kelsey Romeo-Stuppy, Laurent Huber
https://onlinelibrary.wiley.com/doi/abs/10.1111/add.15990
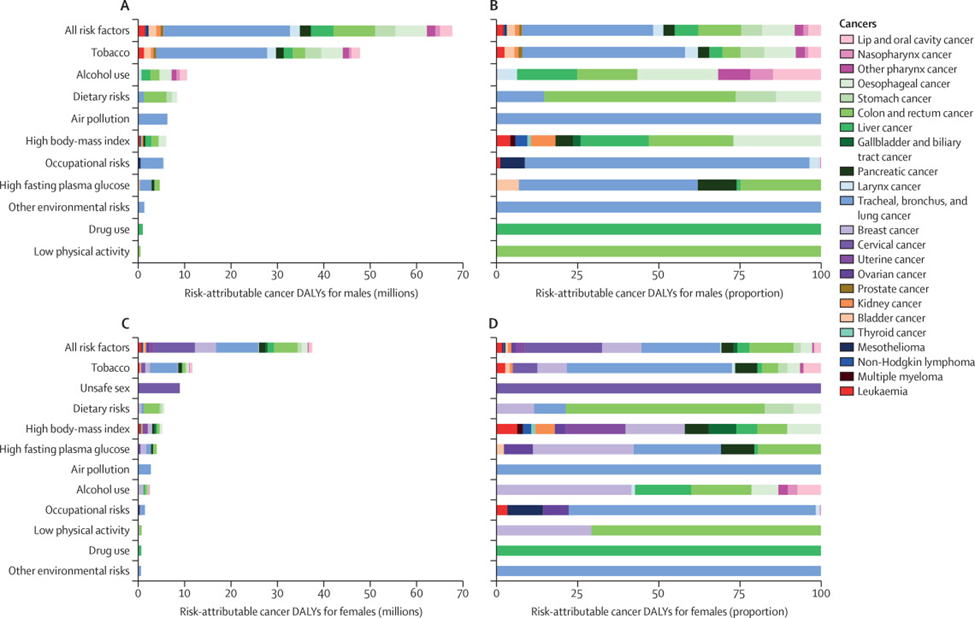
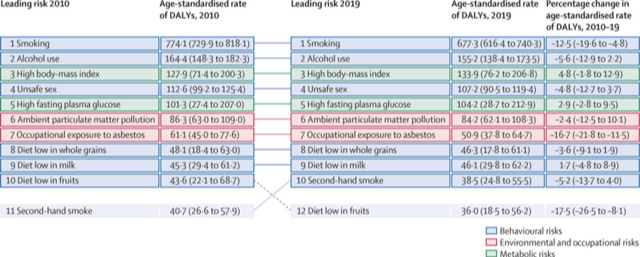
“Globally, there has been substantial progress in reducing exposure to tobacco that can be linked to coordinated international and national prevention efforts. Interventions through taxation and regulatory policies for tobacco smoking, including smoke-free policies, increased tobacco taxes, and advertisement bans guided by the WHO Framework Convention on Tobacco Control, have played a major role in these efforts… Smoking continues to be the leading cancer risk factor globally, with other substantial contributors to cancer burden varying around the world.”
The global burden of cancer attributable to risk factors, 2010–19: a systematic analysis for the Global Burden of Disease Study 2019
The Lancet
VOLUME 400, ISSUE 10352, P563-591, AUGUST 20, 2022
Published: August 20, 2022
GBD 2019 Cancer Risk Factors Collaborators
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)01438-6/fulltext
https://www.thelancet.com/action/showPdf?pii=S0140-6736%2822%2901438-6
Related coverage:
Smoking, alcohol, high BMI leading causes of global cancer deaths: Lancet study
Smoking, Alcohol, High BMI Main Causes Of Global Cancer Deaths: Lancet
“Findings pertaining to the effects of tobacco product use on the incidence of SARS-CoV-2 infection are inconsistent. However, evidence supports a role for cigarette smoking in increasing the risk of poor COVID-19 outcomes, including hospital admission, progression in disease severity, and COVID-19-related mortality… A deeper understanding of the links between tobacco product use and disease risk could help to shape public health recommendations and to improve the clinical care of those with a history of tobacco dependence.”
PERSONAL VIEW
Tobacco product use and the risks of SARS-CoV-2 infection and COVID-19: current understanding and recommendations for future research
Lancet Resp Med
Published: August 16, 2022
Neal L Benowitz, Maciej L Goniewicz, Bonnie Halpern-Felsher, Suchitra Krishnan-Sarin, Pamela M Ling, Richard J O'Connor, Mary Ann Pentz, Rose Marie Robertson, Aruni Bhatnagar
https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(22)00182-5/fulltext